Trochleoplasty
in Munich
Surgery for Patellar Instability
A recurrent dislocation of the kneecap can cause significant discomfort and may lead to long-term cartilage damage. In cases of a congenital malformation of the trochlear groove – known as trochlear dysplasia – surgical correction may be necessary. Trochleoplasty is a proven procedure designed to improve patellar tracking and restore long-term stability of the kneecap, reducing the risk of future dislocations.
When Is a Trochleoplasty Necessary?
Trochleoplasty is performed in patients with recurrent patellar dislocations, especially when conservative treatments fail to provide relief. The following symptoms and diagnoses may indicate the need for surgery:
OUR EXPERTISE
Specialists for Trochleoplasty in Munich
Munich Airport Clinic provides optimal conditions for knee surgeries. Trochleoplasty is performed by our experienced specialists, ensuring expert surgical care. Thanks to modern surgical techniques and precise diagnostics, our patients benefit from the best possible treatment outcomes and a faster, more effective recovery.
STEP BY STEP
Procedure of Trochleoplasty Surgery
Trochleoplasty is a surgical procedure that reshapes the trochlea to ensure the kneecap is properly stabilized within the joint.
1. Preoperative Preparation
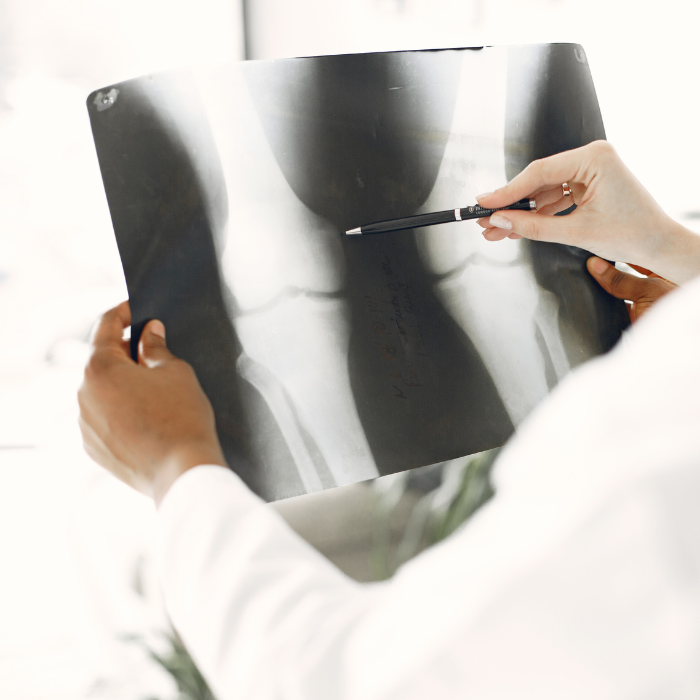
Before the surgery, a comprehensive clinical examination and imaging diagnostics are performed. Based on the patient’s individual knee anatomy, the surgeon determines whether a deepening trochleoplasty is necessary or if an additional stabilization procedure, such as MPFL reconstruction, is required.
Good to know:
MPFL stands for Medial Patellofemoral Ligament, a ligament on the inner side of the knee that stabilizes the kneecap (patella) and prevents it from dislocating outward. In patients with frequent kneecap dislocations, this ligament is often damaged and may need reconstruction.
2. The Surgery
Trochleoplasty is typically performed under general anesthesia and takes about 1–2 hours. The procedure involves the following steps:
Good to know:
A lateral release is a procedure that lengthens tight structures on the outer side of the kneecap. The goal is to reduce tension on the patella, allowing it to return to its natural gliding path without excessive pulling. This comprehensive surgical approach ensures that the kneecap remains stable and properly aligned, minimizing the risk of future dislocations.
3. Immediately After Surgery
Following the procedure, the knee is stabilized with a special brace to ensure optimal healing. Early physiotherapy mobilization typically begins on the first postoperative day. Patients generally stay at our Munich Airport Clinic for one to two days before being discharged.
AFTER THE SURGERY
Rehabilitation and Aftercare
Phase 1 (Up to Week 2) – Protection and Stabilization
After surgery, the knee must be mobilized carefully to ensure optimal healing of the treated structures.
Phase 2 (Weeks 3–6) – Gradual Mobilization
The knee can now gradually bear more weight as healing progresses.
Phase 3 (From Week 12) – Strengthening and Return to Activity
As the knee gains more strength and flexibility, patients can start returning to daily activities and sports.
BENEFITS
Your Benefits at the Munich Airport Clinic
Modern Equipment

Experienced Specialists
Short Waiting Times

Personalized Care
Easy Accessibility
High Hygiene Standards
DIAGNOSIS
Diagnostics: How Is Trochlear Dysplasia Identified?
To reliably diagnose trochlear dysplasia, various imaging techniques are used to assess the structure and alignment of the knee joint.
Dejour Classification:
When Is Surgery Necessary?
The Dejour classification categorizes trochlear dysplasia into four severity levels:
Surgical treatment is advisable from Type B onwards, especially if conservative measures do not provide sufficient patellar stability or if multiple patellar dislocations have already occurred.
A trochleoplasty can significantly improve the quality of life for patients with chronic patellar instability. By correcting the trochlea, the kneecap is stabilized, preventing further dislocations. After a targeted rehabilitation program, most patients can walk pain-free again and return to sports activities.
FAQ
Frequently Asked Questions
About Trochleoplasty
Whether trochleoplasty is required depends on the cause and frequency of the patellar dislocation. If the kneecap frequently dislocates, it may indicate knee joint instability. Occasional dislocations without additional symptoms can often be treated conservatively, such as through physiotherapy to strengthen the muscles.
However, if patellar dislocation occurs regularly or if trochlear dysplasia is present, surgical treatment may be necessary.
The duration of a trochleoplasty procedure depends on the individual condition and any additional necessary procedures. On average, the surgery takes about 1–2 hours. If supplementary measures, such as MPFL reconstruction or lateral release, are required, the surgical time may vary slightly.
The duration of time off work after kneecap surgery depends on individual healing progress and the type of job.
The exact duration of medical leave should be discussed with your treating physician to ensure safe recovery and return to daily activities.